18 Year old female with Bilateral Lower Limb Weakness
Prefinal Practical Case
18 YEAR OLD FEMALE WITH BILATERAL LOWER LIMB WEAKNESS
-January 11, 2022
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
SOWJANYA REDDY PALAKURTHY
ROLL NO. : 130
9th Semester
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE:
18 year old female, house maker by occupation, resident of Masanpally, was brought to the OPD with chief complaints of
- Bilateral lower limb weakness since 1 day.
- Fever since 1 day.
HOPI:
- Pateint was apparently asymptomatic till September,2021.
- In August 2021, she delivered a baby boy. Since then she has been having gradual weakness in both her upper and lower limbs.
- 2 months back, patient experienced an episode of bilateral weakness in upper and lower limbs, that the patient couldn't get up from the bed as soon as she woke up. She was immediately taken to near by hospital in Nalgonda, where she was diagnosed with weakness secondary to hypokalemia and was treated for the same in the hospital for 3 days. She regained the power and was discharged. She was adviced medications. The pateint took prescribed medication for 10 days and abruptly stopped the medication as she was feeling better.
- After stopping medication, patient experienced pain and weakness in the limbs which gradually increased.
- She presented to our hospital on 10th January,2021 with complaints of bilateral lower limb weakness with dragging type of pain in upper limbs. She was not able to get up from the bed as soon as she woke up. She was able to roll on the bed but was unable to sit down or stand. Difficulty in lifting head off the pillow. No difficulty in respiration. No diurnal variation of weakness.
- No fasiculations, no tremors.
- No sensory involvement and no bowel or bladder inconsistence.
- No abnormal movements of limbs.
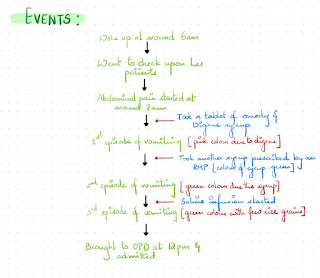
- Patient experienced fever since 9th Jan in the evening. It was high grade and associated with chills and rigor. She was taken to an RMP and an injection was given.
- One episode of vomiting after admission in the hospital. It was non bilious, non projectile and food as content.
DIFFERENTIAL DIAGNOSIS:
- GBS
- Myopathies
- Hypokalemia
- Traumatic neuritis
- Meningitis/encephalitis
- Poliomyelitis
- Myaesthenia gravis
PAST HISTORY:
Not a known case of TB, Asthma, epilepsy, HTN, DM, thyroid abnormalities.
FAMILY HISTORY:
Insignificant.
PERSONAL HISTORY:
- Diet - mixed
- Appetite - decreased since 5 months
- Sleep - adequate
- Bowel and bladder movements- Regular
- No known allergies to drug and food
- No addictions
- Marital status - Married
- Menarche - 13years
- 6/30 cycle
- No clots, no dysmenorrhoea
- G1P1 - Male baby born at 7months of gestation with 1kg weight at birth by normal vaginal delivery.
- She did not breast feed the baby.
GENERAL EXAMINATION:
After taking consent, the pateint was examined in a well lit room.
- The patient is conscious, coherent, cooperative and we'll oriented to time, place and person.
- She is thin built and moderately nourished.
- No pallor, icterus, cyanosis, clubbing, lymphadenopathy, Edema, dehydration.
Vitals at the time of admission :
- Temperature - Afebrile, measured in axilla.
- Pulse - 80bpm regular rhythm, normal in volume. No radio - radio or radio - femoral delay.
- Respiratory rate - 12cpm, regular, thoraco-abdominal.
- Blood pressure - 80/60 mmHg in left arm
- SpO2 - 99% at room air.
- GRBS- 117mg%
CNS examination -
HMF - intact
Cranial nerves - intact
Motor system -. Right. Left
BULK Normal Normal
on inspection and palpation.
POWER
Neck. Good Good
Upper limb 5/5. 5/5
Lower limb 3/5. 3/5(on admission)
4/5. 4/5 (presently)
Trunk muscles. Normal
TONE
Upper limb Normal. Normal
Lower limb. Normal. Normal
REFLEXES
Biceps. +. +
Triceps. +. +
Supinator. +. +
Knee. +. +
Ankle. +. +
Plantar. Flexor. Flexor
Sensory System
- Pain - Normal
- Touch- fine touch - normal
- crude touch - normal
- Temp - normal
- Vibration - normal
- Joint position - normal
Cerebellum
- Finger nose test - normal
- Dysdiadocokinesia - normal
- Tandem walking - normal
- Rombergs test - normal
- Gait - normal
- Signs of meningeal irritation - absent
- Autonomic nervous system - normal
CVS examination-
- Inspection : no visible pulsation , no visible apex beat , no visible scars.
- Palpation: all pulses felt , apex beat felt.
- Percussion: heart borders normal.
- Auscultation:S1, S2 Heard, no added murmurs.
Respiratory system -
- Inspection: shape of chest : normal
- Palpation: trachea normal, chest movement equal on both sides, vocal fremitus felt.
- Percussion: resonant
- Auscultation: Bilateral aur entry present, normal vesicular breathe sounds heard
- Inspection : no engorged veins , no visible peristalsis
- Palpation :soft, non tender, no organomegaly
- Percussion: no free fluid.
- Auscultation: bowel sounds heard
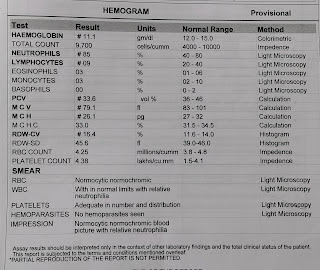
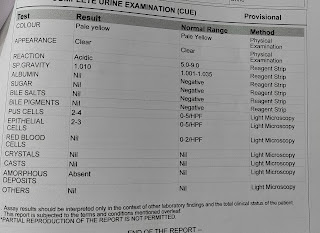
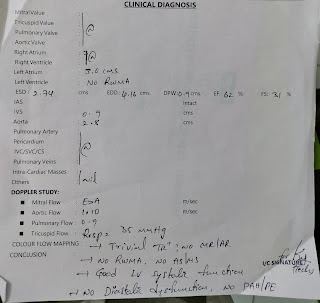
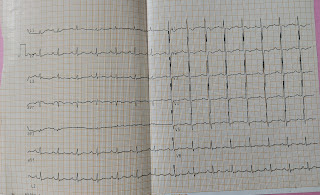
INVESTIGATIONS:
1. Serum electrolytes
2. Blood picture
3. Urine analysis
4. Urinary electrolytes
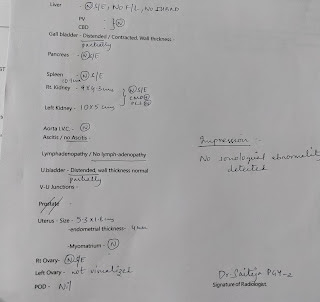
5. USG
6. ECG
7. LFT
8. ABG
9. Echo
10. Serum Urea
Serum electrolytes -
On 11-01-2
- Sodium - 1.1
- Potassium - 2.9
- Chloride - 10
PROVISIONAL DIAGNOSIS:
Paraparesis secondary to hypokalemia
TREATMENT
- IVF NS,RL @75 ML/H
- INJ OPTINUERON 1 AMP IN 100 ML NS IV/O
- INJ PANTOP 40 MG IN/O
- INJ ZOFER 4 MG IN/TI
- SYP POTCHLOR 15 ML IN GLASS OF WATER PO/TI
- MONITOR VITALS 4 TH HOURL
- I/O CHARTING