FINAL EXAMINATION LONG CASE
A 75 YEAR OLD FEMALE WITH DKA AND HTN
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Name : SOWJANYA REDDY PALAKURTHY
Hall Ticket Number : 1701006175
Roll no. - 130
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
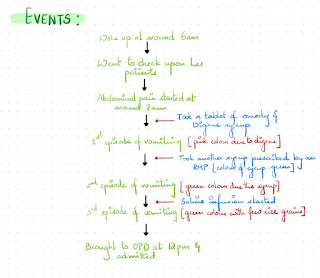
A 75 Year old female, farmer by occupation, resident of Nalgonda , came to casualty on 9th June 2022 with chief complaints of-
CHIEF COMPLAINTS:
1. Nausea and vomitings since morning
2. Giddiness since morning
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 6 years ago then she developed symptoms such a Generalized weakness, headache for which she went to hospital and was diagnosed with Diabetes and Hypertension. She was prescribed medicines for it.
Since 4 days she missed her medications as she went to visit her relatives.
On presentation( 9/06/2022),
she complained of 2-3 episodes of vomiting, non-bilious, non-projectile, followed by giddiness.
She was taken to a local hospital primary, where she was found to have GRBS-394 mg/dl and ketone bodies +ve.
No h/o Chest pain, palpitations, syncopial attacks.
No h/o Shortness of Breath.
No h/o Pain abdomen, burning micturition or loose stools.
DAILY ROUTINE
PAST HISTORY
No history of similar complaints in the past.
Patient is a known case of HTN and DM and is on prescribed medications.
H/o Cataract surgery in right eye 3 years ago and in left eye 2 years ago.
Not a known case of CAD, Bronchial asthma, Epilepsy, TB.
No h/o any previous surgeries.
PERSONAL HISTORY
DIET - Mixed
APPETITE- Normal
SLEEP - Adequate
BOWEL AND BLADDER- Regular
ADDICTIONS - No addictions
No known allergies
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient was examined in a well lit room after taking informed consent.
She is conscious, coherent and cooperative; moderately built and well nourished.
No icterus, clubbing, cyanosis, lymphadenopathy, edema.
VITALS on 9/06/2022
- BLOOD PRESSURE: 230/100 mmHg
- PULSE PRESSURE: 90 Bpm
- RESPIRATORY RATE: 18cpm
- TEMPERATURE: Aferbile
- SpO2: 97% on Room air
- GRBS: 393mg/dl
SYSTEMIC EXAMINATION
1. RESPIRATORY SYSTEM
INSPECTION - No tracheal deviation, Chest bilaterally symmetrical. Thoraco abdominal type of respiration. No dilated veins, pulsations, scars or sinuses.
PALPATION - No tracheal deviation, normal vocal fremitus on both sides.
PERCUSSION - Resonant in all areas.
AUSCULATION - Normal vesicular breath sounds, bilateral air entry present.
2. CARDIOVASCULAR SYSTEM
INSPECTION :- No visible pulsations, no visible apex beat, no visible scars.
PALPATION :- Apex beat felt
AUSCULATION :- Mitral area, tricuspid area, pulmonary area, aortic area - S1, S2 heard.
3. ABDOMINAL EXAMINATION -
INSPECTION - Abdominal distension is present, umbilicus is normal. All quadrants are moving equally with respiration. No visible scars, sinuses, pulsations, engorged veins.
PALPATION - No local rise of temperature or tenderness in all quadrants. No organomegaly.
PERCUSSION - No shifting dullness
AUSCULATION - Bowel sounds and heard, no bruit.
4. CNS -
- Higher mental functions - Normal
- Cranial never functions - Normal
- Sensory system - Sensitive
- Motor system Right Left
LL. 5/5. 5/5
TONE-. UL. Normal. Normal
LL. Normal. Normal
REFLEXES-
Superficial reflexes - Intact
Plantar. Flexion. Flexion
Deep tendon reflexes -
Biceps -. ++. ++
Triceps-. ++. ++
Supinator. ++. ++
Knee. ++. ++
Ankle. ++. ++
GAIT - Normal
- Cerebellar system - Intact
INVESTIGATIONS
1. RANDOM BLOOD SUGAR - 164 mg/dl
2. GLYCATED HEMOGLOBIN (HB1AC)- 6.5%
3. BLOOD UREA - 26 mg/dl
4. SERUM CREATININE- 1.0 mg/dl
5. SERUM ELECTROLYTES-
On 9/06/2022
- Sodium - 139mEq/L
- Potassium - 3.3mEq/L
- Chloride - 98mEq/L
On 11/06/2022
- Sodium - 134mEq/L
- Potassium - 3.6mEq/L
- Chloride - 99mEq/L
On 12/06/2022
- Sodium - 138mEq/L
- Potassium- 3.4mEq/L
- Chloride- 99mEq/L
6. COMPLETE URINE EXAMINATION
On 9/06/2022
- Colour: Pale Yellow
- Appearance: Clear
- Reaction: Acidic
- Specific Gravity : 1.010
- Albumin: ++
- Sugar: ++++
- Bile Salta and Pigments: Nil
- Pus cells: 3-6 /HPF
- Epithelial cells: 2-4 / HPF
- Red blood cell: NIL
- Casts: NIL
7. URINE FOR KETONE BODIES -
On 9/06/2022
Positive
On 11/06/2022
Negative
8. HEMOGRAM
- Hemoglobin: 11.3mg/dl
- Total leucocyte count: 8900cell/cumm
- Neutrophils: 80%
- Lymphocytes:13%
- Eosinophils:02%
- Monocytes:05%
- PCV: 33.7 Volume%
- MCV: 75.4fl
- MCH: 25.3pg
- MCHC: 33.5%
- Platelet Count: 2.67 lakhs/cumm
- RBC Count: 4.47million/cumm
- PBS- Normocytic Normochromic
9. LIVER FUNCTION TESTS:
- Total bilirubin: 0.74mg/dl
- Direct bilirubin: 0.18mg/dl
- Aspartate transaminase: 29IU/L
- Alkaline phosphate: 143IU/L
- Alanine transaminase: 11IU/L
- Total proteins: 7.7g/dl
- Albumin: 4.1g/dl
- A/G ratio: 1.16
10. ABG Analysis
- pH : 7.44
- pCO2 : 30.6mmHg
- pO2. :71.4mmHg
- HCO3:22.6mmol/L
- BEB: -2.0mmol/L
- BEecf: -2.8mmol/L
- TCO2: 40.5VOL
- O2 Count: 18.0vol%
- O2sat:93.8%
11. Seronegative for HIV, HEPATITIS B and C
12. USG- Mild hepatomegaly
13. ECG:
PROVISIONAL DIAGNOSIS
Diabetic Ketosis with Hypertensive Urgency
TREATMENT
9/06/2022
- Intravenous fluids normal saline/ ringer lactate @100ml/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab. NICARDIA 20mg PO/ STAT
- Monitor GRBS, PR, BP, RR CHARTING hourly
- Strict input output charting
10/06/2022
- Intravenous fluids NS 2 @ 100ML/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab TELMA- AM (40/5) mg PO OD
- MONITORING GRBS,BP,PR, RR CHARTING
- Strict Input output charting
11/06/2022
- Intravenous fluids NS 2 @ 75mL/hr
- Injection Human actrapid insuin 10/10/10 and NPH 8/-/8 ,strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab CINOD-T (40/10) mg PO OD
- BP 2nd hourly charting
- Strict input/output charting
12/06/2022
- Injection Human actrapid insulin 12/12/12 and NPH 10/-/10, Strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab CINOD-T (40/10) mg PO OD
- BP 2nd hourly charting
- Strict input/output charting
13/06/2022
- Injection Human actrapid insulin 12/12/12 and NPH 10/-/10, Strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab CINOD-T (40/10) mg PO OD
- BP 2nd hourly charting
- Strict input/output charting